
Protein Intake and Kidney Diseases
Care for your Kidneys’ series
(Brought to you by MOHAN Foundation & Care For Your Kidney Foundation)
Proteins are the building blocks of our body. They help in repair and formation of the tissues, allows metabolic reactions to take place and coordinates bodily functions. The recommended dietary allowance of a healthy average Indian adult is 0.8 to 1 gm per body weight.
Protein is an important nutrient. But if you have kidney disease, you may need to closely watch the protein you eat to prevent protein wastes from building up in your blood. This can help your kidneys work longer. Your doctor will tell you if you need to limit how much protein you eat each day. Decisions are based on your stage of kidney disease, level of nutrition, muscle mass, and other things. It is also important for your protein intake not to be too low. Let your nephrologist and dietitian help you.

Protein and the CKD patient
When protein is ingested, protein waste products are created. Healthy kidneys have millions of nephrons that filter this waste. It’s then removed from the body in the urine.
Unhealthy kidneys lose the ability to remove protein waste and it starts to build up in the blood. Dietary protein intake for patients with CKD is based on the stage of kidney disease, nutrition status and body size. Counselling sessions with a registered dietitian are recommended for planning and monitoring a low- or high-protein diet.
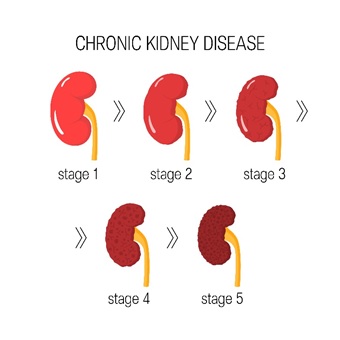
Protein and the stages of chronic kidney disease (CKD)
The five stages of CKD are defined by the glomerular filtration rate (GFR), a measure of how well your kidneys are functioning.
Although stage 4 indicates a severe decrease in kidney function, you’re still able to live without dialysis. The primary focus is keeping you nourished and reducing protein waste build up. Excess protein waste can cause nausea, loss of appetite, vomiting, weakness, taste changes and itching.
If you’re in stages 1, 2, or 3, your protein intake may be limited to 12 to15 percent of your calorie intake each day. This is the same level recommended by the Dietary Reference Intakes (DRIs) for a healthy diet for normal adults. If you’re in stage 4 of CKD, your dietitian may advise you to reduce protein to 10 percent of daily calorie intake.
Protein and ESRD
For patients who are in stage 5 and have kidneys that work at less than 10 percent, dialysis is needed to take over for the failed kidneys or until a kidney transplant is possible.
Dialysis removes protein waste from the blood and a low protein diet is no longer needed. Unfortunately, some amino acids are removed during dialysis. A higher protein intake is needed to replace lost protein.
Diabetes, CKD and protein
If you have CKD as a result of diabetes, your dietitian and doctor will help you manage your diabetes. Good glucose and blood pressure control can help slow down the progression of kidney disease in people with diabetes. Your dietitian will determine the level of protein restriction you need.

Are some proteins better than others?
High protein foods like meat, milk and eggs can be high in fat and cholesterol. If you have high cholesterol or cardiovascular disease, your doctor and dietitian may recommend eating more heart-friendly proteins. Good choices include fish, chicken breast, and low-fat soy products as well as low-fat dairy products.

Phosphorus is a mineral that builds up in the blood as kidney failure progresses. You may be advised to reduce high protein foods that are high in phosphorus, if your level goes above normal. Milk, yogurt, cheese, dried beans and peas, nuts and seeds, peanut butter and some soy products are high in protein and phosphorus.

How is protein managed?
To make sure you’re getting the right amount of protein for your condition, consult your dietitian to get specific guidelines regarding your protein intake. This number will depend on your CKD stage, lab results, body size and other health conditions.
If you’re prescribed a low protein diet, your portions of protein containing foods will be smaller than usual. For the average size person, meat, poultry or fish is limited to about 115 to 170 grams per day.
If I can’t have protein, what can I have?
Although your diet may be limited in high protein foods, you’ll still eat a variety of foods, such as eggs, milk, meat, poultry, fish, fruits, vegetables and grains. Eating adequate calories is important to prevent muscle breakdown and weight loss. You may be advised to eat more healthy fats, such as olive oil, or take supplements to help you get enough calories.
Depending on your condition, you may also need to limit sodium, potassium or phosphorus. This is determined by your blood pressure and your laboratory values. Consult you dietitian.

